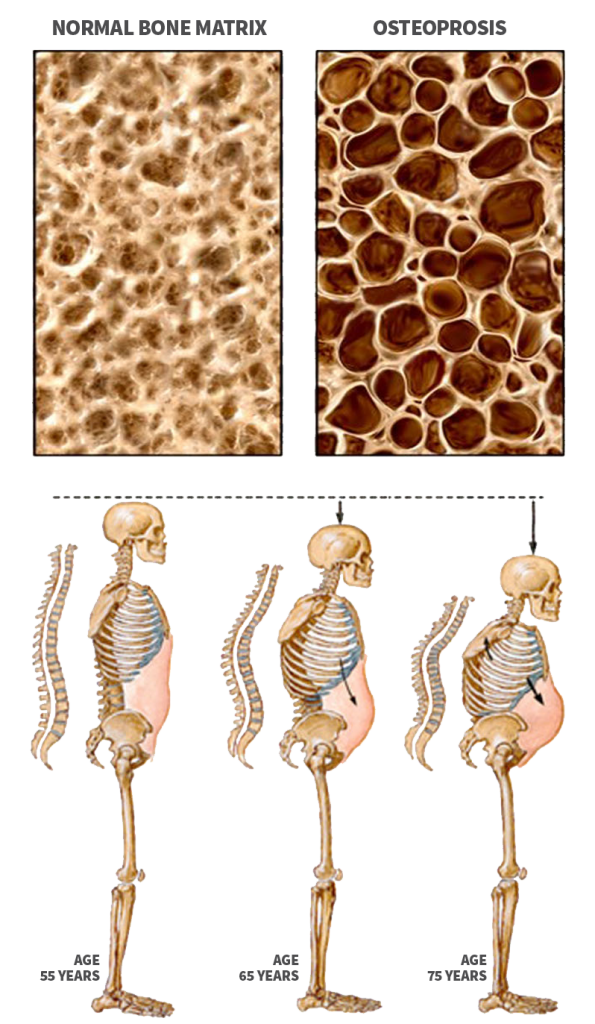
Osteoporosis is a bone disease characterized by decrease in bone mass and density resulting in brittle, fragile bones that are more susceptible to fractures, even without injury. The condition most commonly develops in elderly women. Osteoporosis may cause no symptoms in the early stage of the disease. Later as the condition progresses it may cause the following symptoms:
- Low back pain and neck pain due to fractures of the spinal bones.
- Dull pain in the bones accompanied by tenderness.
- Loss of the height of the spine giving a stooped posture or hump.
- Fractures from minimal trauma.
Multiple risk factors for developing osteoporosis have been identified. These include smoking, kidney disease, hyperthyroidism, autoimmune conditions such as rheumatoid arthritis and lupus, COPD, chronic steroid use, inflammatory bowel disease, gastrointestinal mal-absorption diseases, etc.
The diagnosis of osteoporosis based on the medical history, physical examination and a bone density test. Bone mineral density test is a painless, non invasive and safe method of measuring bone density.
TREATMENT
There are different treatment options for osteoporosis:
- Diet: Consume a balanced diet rich in calcium and vitamin D. The National Osteoporosis Foundation Guidelines recommend a daily intake of calcium at 1200-1500 mg daily and vitamin D at 800-1,000 IU daily. Depending on the patient’s vitamin D level in the blood, additional vitamin D3 may be warranted.
- Exercise: Regular exercises can decrease the risk of developing bone fractures in people with osteoporosis. Your doctor may recommend weight bearing exercises such as walking and light weight lifting.
- Medications: Medications such as alendronate, risedronate, raloxifene, ibandronate, and are used to strengthen bones, decrease bone loss and decrease the risk of fractures.
For patients who cannot tolerate oral medications, injectable alternatives like Prolia and Forteo are also available.